Plasmodium vivax
| Plasmodium vivax | |
|---|---|
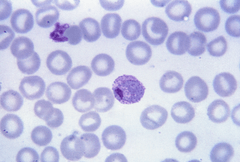 | |
| Mature P. vivax trophozoite | |
| Scientific classification | |
| (unranked): | SAR |
| Phylum: | Apicomplexa |
| Class: | Aconoidasida |
| Order: | Haemosporida |
| Family: | Plasmodiidae |
| Genus: | Plasmodium |
| Species: | P. vivax |
| Binomial name | |
| Plasmodium vivax (Grassi & Feletti, 1890) | |
| Synonyms[1] | |
|
Haemamoeba vivax Grassi and Feletti, 1890 | |
Plasmodium vivax is a protozoal parasite and a human pathogen. The most frequent and widely distributed cause of recurring (Benign tertian) malaria, P. vivax is one of the five species of malaria parasites that commonly infect humans.[2] It is less virulent than Plasmodium falciparum, the deadliest of the five, but vivax malaria can lead to severe disease and death due to splenomegaly (a pathologically enlarged spleen).[3][4] P. vivax is carried by the female Anopheles mosquito, since it is only the female of the species that bite.
Health
The World Health Organization (WHO) is drawing up a plan to address vivax malaria, due out in 2015.
Epidemiology
P. vivax was found mainly in the United States, Latin America, and in some parts of Africa.[5][6] More recently it became a plague of low- and middle-income countries, except those in sub-Saharan Africa, where the P. vivax map has a conspicuous hole. Overall it accounts for 65% of malaria cases in Asia and South America.[7] It is logical that plasmodium vivax is found there where humans and mosquito population are high. It is uncommon in cooler areas.
As overall malaria rates fall in a region, its proportion of cases increases.[7] It has been estimated that 2.5 billion people are at risk of infection with this organism.[8]
Although the Americas contribute 22% of the global area at risk, high endemic areas are generally sparsely populated and the region contributes only 6% to the total population at risk. In Africa, the widespread lack of the Duffy antigen in the population has ensured that stable transmission is constrained to Madagascar and parts of the Horn of Africa. It contributes 3.5% of global population at risk. Central Asia is responsible for 82% of global population at risk with high endemic areas coinciding with dense populations particularly in India and Myanmar. South East Asia has areas of high endemicity in Indonesia and Papua New Guinea and overall contributes 9% of global population at risk.[9]
P. vivax is carried by at least 71 mosquito species. Many vivax vectors live happily in temperate climates—as far north as Finland. Some prefer to bite outdoors or during the daytime, hampering the effectiveness of indoor insecticide and bed nets. Several key vector species have yet to be grown in the lab for closer study, and insecticide resistance is unquantified.[7]
Clinical presentation
Pathogenesis results from rupture of infected red blood cells, leading to fever. Infected red blood cells may also stick to each other and to walls of capillaries. Vessels plug up and deprive tissues of oxygen. Infection may also cause the spleen to enlarge. [10]
Unlike P. falciparum, P. vivax can populate the bloodstream with sexual-stage parasites—the form picked up by mosquitoes on their way to the next victim—even before a patient shows symptoms. Consequently, prompt treatment of symptomatic patients doesn't necessarily help stop an outbreak, as it does with falciparum malaria, in which fevers occur as sexual stages develop. Even when symptoms appear, because they are usually not immediately fatal, the parasite continues to multiply.[7]
The parasite can go dormant in the liver for days to years, causing no symptoms and remaining undetectable in blood tests. They form what are called hypnozoites (the name derives from "sleeping organisms"), a small form that nestles inside an individual liver cell. The hypnozoites allow the parasite to survive in more temperate zones, where mosquitoes bite only part of the year.[7]
A single infectious bite can trigger six or more relapses a year, leaving sufferers more vulnerable to other diseases. Other infectious diseases, including falciparum malaria, appear to trigger relapses.[7]
Prevention
The main way to prevent malaria is through vector control. There are mostly three main forms that the vector can be controlled: (1)insecticide-treated mosquito nets, (2)indoor residual spraying and (3)antimalarial drugs. Long-lasting insecticidal nets (LLNs) are the preferred method of control because it is the most cost effective. The WHO is currently strategizing how to ensure that the net is properly maintained to protect people at risk. The second option is indoor residual spraying and has been proven effective if at least 80% of the homes are sprayed. However, such method is only effective for 3-6months. A drawback to these two methods, unfortunately, is that mosquito resistance against these insecticides has risen. National malaria control efforts are undergoing rapid changes to ensure the people are given the most effective method of vector control. Lastly, antimalarial drugs can also be used to prevent infection from developing into a clinical disease. However, there has also been an increase resistance to antimalarial medicine.[11]
Diagnosis
P. vivax and P. ovale that has been sitting in EDTA for more than 30 minutes before the blood film is made will look very similar in appearance to P. malariae, which is an important reason to warn the laboratory immediately when the blood sample is drawn so they can process the sample as soon as it arrives. Blood films are preferably made within 30 minutes of the blood draw and must certainly be made within an hour of the blood being drawn. Diagnosis can be done with the strip fast test of antibodies.
Treatment
Chloroquine remains the treatment of choice for vivax malaria,[12] except in Indonesia's Irian Jaya (Western New Guinea) region and the geographically contiguous Papua New Guinea, where chloroquine resistance is common (up to 20% resistance). Chloroquine resistance is an increasing problem in other parts of the world, such as Korea[13] and India.
When chloroquine resistance is common or when chloroquine is contraindicated, then artesunate is the drug of choice, except in the U.S., where it is not approved for use.[14] Where an artemisinin-based combination therapy has been adopted as the first-line treatment for P. falciparum malaria, it may also be used for P. vivax malaria in combination with primaquine for radical cure.[12] An exception is artesunate plus sulfadoxine-pyrimethamine (AS+SP), which is not effective against P. vivax in many places.[12] Mefloquine is a good alternative and in some countries is more readily available.[15] Atovaquone-proguanil is an effective alternative in patients unable to tolerate chloroquine.[16] Quinine may be used to treat vivax malaria but is associated with inferior outcomes.
32–100% of patients will relapse following successful treatment of P. vivax infection if a radical cure (eradication of liver stages) is not given.[17][18]
Eradication of the liver stages is achieved by giving primaquine. Patients with glucose-6-phosphate dehydrogenase risk haemolysis.[19] G6PD is an enzyme important for blood chemistry. No field-ready test is available.[7] Recently, this point has taken particular importance for the increased incidence of vivax malaria among travelers.[20] At least a 14-day course of primaquine is required for the radical treatment of P. vivax.[12]
Tafenoquine
In 2013 a Phase IIb trial was completed that he studied a single-dose alternative drug named tafenoquine.[21] It is an 8-aminoquinoline, of the same family as primaquine,[22] developed by researchers at the Walter Reed Army Institute of Research in the 1970s and tested in safety trials. It languished, however, until the push for malaria elimination sparked new interest in primaquine alternatives.[7]
Among patients who received a 600-mg dose, 91% were relapse-free after 6 months. Among patients who received primaquine, 24% relapsed within 6 months. "The data are absolutely spectacular," Wells says. Ideally, he says, researchers will be able to combine the safety data from the Army's earlier trials with the new study in a submission to the U.S. Food and Drug Administration for approval. Like primaquine, tafenoquine causes hemolysis in people who are G6PD deficient.[7]
In 2013 researchers produced cultured human "microlivers" that supported liver stages of both P. falciparum and P. vivax and may have also created hypnozoites.[7]
Eradication
Mass-treating populations with a primaquine can kill the hypnozoites, exempting those with G6PD deficiency. However, the standard regimen requires a daily pill for 14 days across an asymptomatic population.
Korea
P. vivax is the only indigenous malaria parasite on the Korean peninsula. In the years following the Korean War (1950–53), malaria-eradication campaigns successfully reduced the number of new cases of the disease in North Korea and South Korea. In 1979, World Health Organization declared the Korean peninsula vivax malaria-free, but the disease unexpectedly re-emerged in the late 1990s and still persists today. Several factors contributed to the re-emergence of the disease, including reduced emphasis on malaria control after 1979, floods and famine in North Korea, emergence of drug resistance and possibly global warming. Most cases are identified along the Korean Demilitarized Zone. As such, vivax malaria offers the two Koreas an opportunity to work together on an important health problem that affects both countries.[23][24]
Biology
Life cycle
Like all malaria parasites, P. vivax has a complex life cycle. It infects a definitive insect host, where sexual reproduction occurs, and an intermediate vertebrate host, where asexual amplification occurs. In P. vivax, the definitive hosts are Anopheles mosquitoes (also known as the vector), while humans are the intermediate asexual hosts. During its life cycle, P. vivax assumes many different physical forms.
Asexual forms:
- Sporozoite: Transfers infection from mosquito to human
- Immature trophozoites (Ring or signet-ring shaped), about 1/3 of the diameter of a RBC.
- Mature trophozoites: Very irregular and delicate (described as amoeboid); many pseudopodial processes seen. Presence of fine grains of brown pigment (malarial pigment) or hematin probably derived from the haemoglobin of the infected red blood cell.
- Schizonts (also called meronts): As large as a normal red cell; thus the parasitized corpuscle becomes distended and larger than normal. There are about sixteen merozoites.
Sexual forms:
- Gametocytes: Round. P. vivax gametocytes are commonly found in human peripheral blood at about the end of the first week of parasitemia.
- Gametes: Formed from gametocytes in mosquitoes.
- Zygote: Formed from combination of gametes
- Oocyst: Contains zygote, develops into sporozoites
Human infection
P. vivax human infection occurs when an infected mosquito feeds on a human. During feeding, the mosquito injects saliva to prevent blood clotting (along with sporozoites), thousands of sporozoites are inoculated into human blood; within a half-hour the sporozoites reach the liver. There they enter hepatic cells, transform into the trophozoite form and feed on hepatic cells, and reproduce asexually. This process gives rise to thousands of merozoites (plasmodium daughter cells) in the circulatory system and the liver.
The incubation period of human infection usually ranges from ten to seventeen days and sometimes up to a year. Persistent liver stages allow relapse up to five years after elimination of red blood cell stages and clinical cure.
Liver stage
The P. vivax sporozoite enters a hepatocyte and begins its exoerythrocytic schizogony stage. This is characterized by multiple rounds of nuclear division without cellular segmentation. After a certain number of nuclear divisions, the parasite cell will segment and merozoites are formed.
There are situations where some of the sporozoites do not immediately start to grow and divide after entering the hepatocyte, but remain in a dormant, hypnozoite stage for weeks or months. The duration of latency is variable from one hypnozoite to another and the factors that will eventually trigger growth are not known; this explains how a single infection can be responsible for a series of waves of parasitaemia or "relapses". Different strains of P. vivax have their own characteristic relapse pattern and timing. The earlier stage is exo-erythrocytic generation.
Erythrocytic cycle
P. vivax preferentially penetrates young red blood cells (reticulocytes). In order to achieve this, merozoites have two proteins at their apical pole (PvRBP-1 and PvRBP-2). The parasite uses the Duffy blood group antigens (Fy6) to penetrate red blood cells. This antigen does not occur in the majority of humans in West Africa [phenotype Fy (a-b-)]. As a result, P. vivax occurs less frequently in West Africa.[25]
The parasitised red blood cell is up to twice as large as a normal red cell and Schüffner's dots (also known as Schüffner's stippling or Schüffner's granules) are seen on the infected cell's surface. Schüffner's dots have a spotted appearance, varying in color from light pink, to red, to red-yellow, as coloured with Romanovsky stains. The parasite within it is often wildly irregular in shape (described as "amoeboid"). Schizonts of P. vivax have up to twenty merozoites within them. It is rare to see cells with more than one parasite within them. Merozoites will only attach to immature blood cell (reticulocytes) and therefore it is unusual to see more than 3% of all circulating erythrocytes parasitised.
Mosquito stage
Parasite life cycle in mosquitoes includes all stages of sexual reproduction:
- Infection and Gametogenesis
- Microgametes
- Macrogametes
- Fertilization
- Ookinite
- Oocyst
- Sporogony
Mosquito Infection and Gamete Formation
When a female Anopheles mosquito bites an infected person, gametocytes and other stages of the parasite are transferred to the mosquito stomach. Gametocytes ultimately develop into gametes, a process known as gametogony.
Microgametocytes become very active, and their nuclei undergo fission (i.e amitosis) to each give 6-8 daughter nuclei, which becomes arranged at the periphery. The cytoplasm develops long thin flagella like projections, then a nucleus enter into each one of these extensions. These cytoplasmic extensions later break off as mature male gametes (microgametes). This process of formation of flagella-like microgametes or male gametes is known as exflagellation. Macrogametocytes show very little change. They develop a cone of reception at one side and becomes mature as macrogametocytes (female gametes).
Fertilization
Male gametes move actively in the stomach of mosquitoes in search of female gametes. Male gametes then enter into female gametes through the cone of reception. The complete fusion of 2 gametes results in the formation of zygote. Here, fusion of 2 dissimilar gametes occurs, known as anisogamy.
The zygote remains inactive for sometime but it soon elongates, becomes vermiform (worm-like) and motile. It is now known as ookinete. The pointed ends of ookinete penetrate the stomach wall and come to lie below its outer epithelial layer. Here the zygote becomes spherical and develops a cyst wall around itself. The cyst wall is derived partly from the stomach tissues and partly produced by the zygote itself. At this stage, the zygote is known as an oocyst. The oocyst absorbs nourishment and grows in size. Oocysts protrude from the surface of stomach, giving it a blistered appearance. In a highly infected mosquito, as many as 1000 oocysts may be seen.
Sporogony
The oocyst nucleus divides repeatedly to form large number of daughter nuclei. At the same time, the cytoplasm develops large vacuoles and forms numerous cytoplasmic masses. These cytoplasmic masses then elongate and a daughter nuclei migrates into each mass. The resulting sickle-shaped bodies are known as sporozoites. This phase of asexual multiplication is known as sporogony and is completed in about 10–21 days. The oocyst then bursts and sporozoites are released into the body cavity of mosquito. Sporozoites eventually reach the salivary glands of mosquito via its hemolymph. The mosquito now becomes infectious. Salivary glands of a single infected mosquito may contain as many as 200,000 sporozoites. When the mosquito bites a healthy person, thousands of sporozoites are infected into the blood along with the saliva and the cycle starts again.
Taxonomy
P. vivax can be divided into two clades one that appears to have origins in the Old World and a second that originated in the New World.[26] The distinction can be made on the basis of the structure of the A and S forms of the rRNA. A rearrangement of these genes appears to have occurred in the New World strains. It appears that a gene conversion occurred in an Old World strain and this strain gave rise to the New World strains. The timing of this event has yet to be established.
At present both types of P. vivax circulate in the Americas. The monkey parasite - Plasmodium simium - is related to the Old World strains rather than to the New World strains.
A specific name - Plasmodium collinsi - has been proposed for the New World strains but this suggestion has not been accepted to date.
Miscellaneous
It has been suggested that P. vivax has horizontally acquired genetic material from humans. [27]
Plasmodium vivax is not known to have a particular gram stain (negative vs. positive) and may appear as either.
Therapeutic use
P. vivax was used between 1917 and the 1940s for malariotherapy, that is, to create very high fevers to combat certain diseases such as tertiary syphilis. In 1917, the inventor of this technique, Julius Wagner-Jauregg, received the Nobel Prize in Physiology or Medicine for his discoveries. However, the technique was dangerous, killing about 15% of patients, so it is no longer in use.[28]
See also
References
- ↑ Coatney GR, Collins WE, Warren M, Contacos PG (1971). "5 Plasmodium vivax (Grassi and Feletti, 1890)". The primate malarias. Division of Parasitic Disease, CDC. p. 43.
- ↑ White, NJ (Jan 15, 2008). "Plasmodium knowlesi: the sixth human malaria parasite.". Clinical Infectious Diseases. 46 (2): 172–3. doi:10.1086/524889. PMID 18171246.
- ↑ Baird, J. Kevin (1 November 2007). "Neglect of Plasmodium vivax malaria". Trends in Parasitology. 23 (11): 533–539. doi:10.1016/j.pt.2007.08.011.
- ↑ Anstey, NM; Douglas, NM; Poespoprodjo, JR; Price, RN (2012). "Plasmodium vivax: clinical spectrum, risk factors and pathogenesis.". Advances in parasitology. 80: 151–201. doi:10.1016/b978-0-12-397900-1.00003-7. PMID 23199488.
- ↑ "Biology: Malaria Parasites". Malaria. CDC. 2004-04-23. Retrieved 2008-09-30.
- ↑ Lindsay SW, Hutchinson RA (2006). "Malaria and deaths in the English marshes—Authors' reply". Lancet. 368 (9542): 1152. doi:10.1016/S0140-6736(06)69467-1.
- 1 2 3 4 5 6 7 8 9 10 Vogel, G. (2013). "The Forgotten Malaria". Science. 342 (6159): 684–687. doi:10.1126/science.342.6159.684.
- ↑ Gething PW, Elyazar IR, Moyes CL, Smith DL, Battle KE, Guerra CA, Patil AP, Tatem AJ, Howes RE, Myers MF, George DB, Horby P, Wertheim HF, Price RN, Müeller I, Baird JK, Hay SI (2012). "A long neglected world malaria map: Plasmodium vivax endemicity in 2010". PLoS Negl Trop Dis. 6 (9): e1814. doi:10.1371/journal.pntd.0001814. PMC 3435256
 . PMID 22970336.
. PMID 22970336. - ↑ Battle, KE; Gething, PW; Elyazar, IR; Moyes, CL; Sinka, ME; Howes, RE; Guerra, CA; Price, RN; Baird, KJ; Hay, SI (2012). "The global public health significance of Plasmodium vivax.". Advances in parasitology. 80: 1–111. doi:10.1016/b978-0-12-397900-1.00001-3. PMID 23199486.
- ↑
- ↑ World Health Organization http://www.who.int/mediacentre/factsheets/fs094/en/. Retrieved 20 October 2016. Missing or empty
|title=(help) - 1 2 3 4 Guidelines for the treatment of malaria, second edition Authors: WHO. Number of pages: 194. Publication date: 2010. Languages: English. ISBN 978-92-4-154792-5
- ↑ Lee KS, Kim TH, Kim ES, et al. (1 February 2009). "Chloroquine-resistant Plasmodium vivax in the Republic of Korea". Am J Trop Med Hyg. 80 (2): 215–217. PMID 19190216.
- ↑ Pukrittayakamee S, et al. (2000). "Therapeutic Responses to Different Antimalarial Drugs in Vivax Malaria". Antimicrob Agents Chemother. 44 (6): 1680–5. doi:10.1128/AAC.44.6.1680-1685.2000. PMC 89932
 . PMID 10817728.
. PMID 10817728. - ↑ Maguire JD, Krisin, Marwoto H, Richie TL, Fryauff DJ, Baird JK (2006). "Mefloquine is highly efficacious against chloroquine-resistant Plasmodium vivax malaria and Plasmodium falciparum malaria in Papua, Indonesia". Clin Infect Dis. 42 (8): 1067–72. doi:10.1086/501357. PMID 16575721.
- ↑ Looareesuwan S, Wilairatana P, Glanarongran R, et al. (1999). "Atovaquone and proguanil hydrochloride followed by primaquine for treatment of Plasmodium vivax malaria in Thailand". Trans. R. Soc. Trop. Med. Hyg. 93 (6): 637–40. doi:10.1016/S0035-9203(99)90079-2. PMID 10717754.
- ↑ Wiselogle FY (1943). J.W. Edwards, ed. A survey of antimalarial drugs, 1941–1945 (2 vols.). Ann Arbor, Michigan.
- ↑ Alving AS, Hankey DD, Coatney GR, et al. (1953). "Korean vivax malaria. II. Curative treatment with pamaquine and primaquine". Am J Trop Med Hyg. 6 (6): 970–6. PMID 13104805.
Adak T, Sharma VP, Orlov VS (1998). "Studies on the Plasmodium vivax relapse pattern in Delhi, India". Am J Trop Med Hyg. 59 (1): 175–9. PMID 9684649. - ↑ Baird JK, Hoffman SL (November 2004). "Primaquine therapy for malaria". Clin. Infect. Dis. 39 (9): 1336–45. doi:10.1086/424663. PMID 15494911.
- ↑ Saleri N, Gulletta M, Matteelli A, et al. (2006). "Acute respiratory distress syndrome in Plasmodium vivax malaria in traveler returning from Venezuela". J Travel Med. 13 (2): 112–3. doi:10.1111/j.1708-8305.2006.00024.x. PMID 16553597.
- ↑ Llanos-Cuentas, A.; Lacerda, M. V.; Rueangweerayut, R.; Krudsood, S.; Gupta, S. K.; Kochar, S. K.; Arthur, P.; Chuenchom, N.; Möhrle, J. R. J.; Duparc, S.; Ugwuegbulam, C.; Kleim, J. R. P.; Carter, N.; Green, J. A.; Kellam, L. (2013). "Tafenoquine plus chloroquine for the treatment and relapse prevention of Plasmodium vivax malaria (DETECTIVE): A multicentre, double-blind, randomised, phase 2b dose-selection study". The Lancet. 383: 1049–1058. doi:10.1016/S0140-6736(13)62568-4.
- ↑ "Tafenoquine". MMV. Retrieved 2014-02-17.
- ↑ For Re-Eradication of Malaria in Korea, Korea Times 05-19-2008
- ↑ The Korean War Against Malaria, Far Eastern Economic Review 07-09-2008
- ↑ Van den Enden J. "Illustrated Lecture Notes on Tropical Medicine". Illustrated Lecture Notes on Tropical Medicine. Retrieved 2015-11-01.
- ↑ Li J, Collins WE, Wirtz RA, Rathore D, Lal A, McCutchan TF (2001). "Geographic subdivision of the range of the malaria parasite Plasmodium vivax". Emerging Infect. Dis. 7 (1): 35–42. doi:10.3201/eid0701.700035. PMC 2631686
 . PMID 11266292.
. PMID 11266292. - ↑ "Evidence of Massive Horizontal Gene Transfer Between Humans and Plasmodium vivax : Nature Precedings". Precedings.nature.com. Retrieved 2014-02-17.
- ↑ Gretchen Vogel (8 November 2013). "Malaria as a Lifesaving Therapy". Science. 342 (6159): 686. doi:10.1126/science.342.6159.686. PMID 24202157.