Posterior reversible encephalopathy syndrome
| Posterior reversible encephalopathy syndrome | |
|---|---|
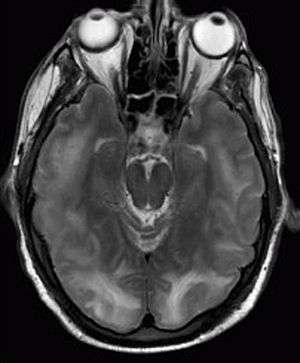 | |
| Posterior reversible encephalopathy syndrome visible on magnetic resonance imaging as multiple cortico-subcortical areas of T2-weighted hyperintense (white) signal involving the occipital and parietal lobes bilaterally and pons. | |
| Classification and external resources | |
| Specialty | neurology |
| ICD-10 | G93.4 |
| ICD-9-CM | 348.39 |
| DiseasesDB | 10460 |
| MeSH | D054038 |
Posterior reversible encephalopathy syndrome (PRES), also known as reversible posterior leukoencephalopathy syndrome (RPLS), is a syndrome characterized by headache, confusion, seizures and visual loss. It may occur due to a number of causes, predominantly malignant hypertension, eclampsia and some medical treatments. On magnetic resonance imaging (MRI) of the brain, areas of edema (swelling) are seen. The symptoms tend to resolve after a period of time, although visual changes sometimes remain.[1][2] It was first described in 1996.[3]
Signs and symptoms
Typical symptoms of PRES, listed according to prevalence, include: altered mental status (encephalopathy), seizure, and headache. Less commonly there may be visual disturbances, focal neurologic signs, and status epilepticus.[4][5]
Causes
Several factors appear to play a role in the pathogenesis of PRES, including medications that suppress the function of the immune system (immunosuppressive medications), kidney failure, eclampsia, severe high blood pressure,[4] and systemic lupus erythematosus.[6]
Diagnosis
The diagnosis is typically made clinically, with supportive findings on magnetic resonance imaging of the brain; this may show hyperintensities on T2-weighed imaging. Three different patterns have been described on MRI imaging including: superior frontal sulcus pattern, dominant parieto-occipital pattern, and holohemispheric watershed pattern.[5][7]
Treatment
The treatment of PRES depends on the underlying cause. For instance, if the main problem is high blood pressure, blood pressure control will accelerate the resolution of the abnormalities. If the likely cause is medication, the withdrawal of the drug in question is needed.[8] Additionally, if the presentation is complicated by seizures, treatment with anti-epileptic medication is suggested.[5]
Prognosis
Many cases resolve within 1–2 weeks of controlling the blood pressure and eliminating the inciting factor. However, some cases are longer-lasting, and may involve permanent neurologic dysfunction in the form of visual changes and seizures among others.[5] Though uncommon, death may occur with progressive swelling of the brain (cerebral edema), compression of the brainstem, increased intracranial pressure, or a bleed in the brain (intracerebral hemorrhage).[5] PRES may recur in about 5-10% of cases; this occurs more commonly in cases precipitated by hypertension as opposed to other factors (medications, etc.).[5]
Epidemiology
The number cases of PRES that occur each year is not known. It may be somewhat more common in females.
See also
References
- ↑ Garg RK (January 2001). "Posterior leukoencephalopathy syndrome". Postgrad Med J. 77 (903): 24–8. doi:10.1136/pmj.77.903.24. PMC 1741870
 . PMID 11123390.
. PMID 11123390. - ↑ Pula JH, Eggenberger E (November 2008). "Posterior reversible encephalopathy syndrome". Curr Opin Ophthalmol. 19 (6): 479–84. doi:10.1097/ICU.0b013e3283129746. PMID 18854692.
- ↑ Hinchey J, Chaves C, Appignani B, Breen J, Pao L, Wang A, Pessin M, Lamy C, Mas J, Caplan L (1996). "A reversible posterior leukoencephalopathy syndrome.". N Engl J Med. 334 (8): 494–500. doi:10.1056/NEJM199602223340803. PMID 8559202.
- 1 2 Rajasekhar, A.; George, T. J. (November 2007). "Gemcitabine-Induced Reversible Posterior Leukoencephalopathy Syndrome: A Case Report and Review of the Literature". The Oncologist. 12 (11): 1332–1335. doi:10.1634/theoncologist.12-11-1332. PMID 18055853.
- 1 2 3 4 5 6 Fugate, Jennifer E.; Rabinstein, Alejandro A. (2015-09-01). "Posterior reversible encephalopathy syndrome: clinical and radiological manifestations, pathophysiology, and outstanding questions". The Lancet Neurology. 14 (9): 914–925. doi:10.1016/S1474-4422(15)00111-8. ISSN 1474-4465. PMID 26184985.
- ↑ Kur, JK; Esdaile, JM (November 2006). "Posterior reversible encephalopathy syndrome--an underrecognized manifestation of systemic lupus erythematosus.". The Journal of Rheumatology. 33 (11): 2178–83. PMID 16960925.
- ↑ Peter P, George A. Posterior reversible encephalopathy syndrome and the pediatric population. J Pediatr Neurosci 2012;7:136-8.
- ↑ Pedraza, R; Marik PE; Varon J (November 2009). "Posterior Reversible Encephalopathy Syndrome: A Review" (PDF). Critical Care and Shock. 12: 135–143.