Cervical cancer staging


Cervical cancer staging is the assessment of cervical cancer to decide how far the disease has progressed. Cancer staging generally runs from stage 0, which is pre-cancerous or non-invasive, to stage 4, in which the cancer has spread throughout a significant part of the body. As a general rule, Stage 0 is easily cured and Stage 4 is incurable.
Cervical cancer is staged by the International Federation of Gynecology and Obstetrics (FIGO) staging system, which is based on clinical examination, rather than surgical findings. It allows only the following diagnostic tests to be used in determining the stage: palpation (feeling with the fingers), inspection, colposcopy, endocervical curettage, hysteroscopy, cystoscopy, proctoscopy, intravenous urography, and X-ray examination of the lungs and skeleton, and cervical conization.
Stages
- Stage 0
- The carcinoma is confined to the surface layer (cells lining) of the cervix. Also called carcinoma in situ (CIS).
- Stage I
- The carcinoma has grown deeper into the cervix, but has not spread beyond it (extension to the corpus would be disregarded). Stage One is subdivided as follows:
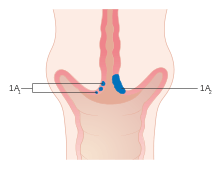
- IA Invasive carcinoma which can be diagnosed only by microscopy, with deepest invasion <5 mm and the largest extension <7 mm
- IA-1 Measured stromal invasion of <3.0 mm in depth and extension of <7.0 mm
- IA-2 Measured stromal invasion of >3.0 mm and not >5.0 mm with an extension of not >7.0 mm
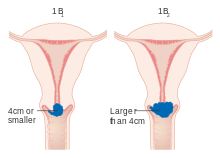
- IB Clinically visible lesions limited to the cervix uteri or pre-clinical cancers greater than stage IA
- IB-1 Clinically visible lesion <4.0 cm in greatest dimension
- IB-2 Clinically visible lesion >4.0 cm in greatest dimension
- IA Invasive carcinoma which can be diagnosed only by microscopy, with deepest invasion <5 mm and the largest extension <7 mm
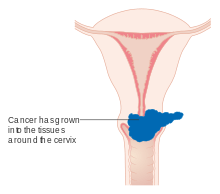
- Stage II
- Cervical carcinoma invades beyond the uterus, but not to the pelvic wall or to the lower third of the vagina
- IIA Without parametrial invasion
- IIA-1 Clinically visible lesion <4.0 cm in greatest dimension
- IIA-2 Clinically visible lesion >4.0 cm in greatest dimension
- IIB With obvious parametrial invasion
- IIA Without parametrial invasion
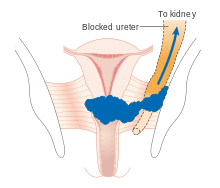
- Stage III
- The tumour extends to the pelvic wall and/or involves lower third of the vagina and/or causes hydronephrosis or non-functioning kidney
- IIIA Tumour involves lower third of the vagina, with no extension to the pelvic wall
- IIIB Extension to the pelvic wall and/or hydronephrosis or non-functioning kidney
- Stage IV
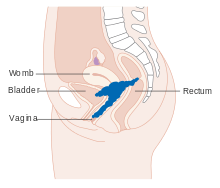
- The carcinoma has extended beyond the true pelvis or has involved (biopsy proven) the mucosa of the bladder or rectum. A bullous oedema, as such, does not permit a case to be allotted to Stage IV
- IVA Spread of the growth to adjacent organs
- IVB Spread to distant organs[1]
References
Diagrams
-
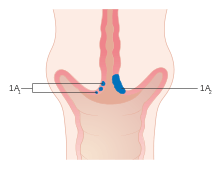
Stage 1A cervical cancer
-
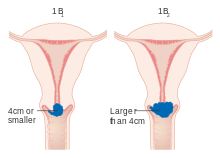
Stage 1B cervical cancer
-

Stage 2A cervical cancer
-
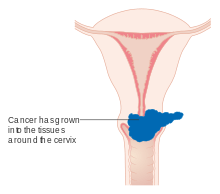
Stage 2B cervical cancer
-
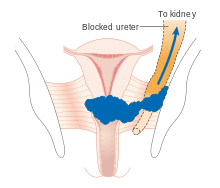
Stage 3B cervical cancer
-
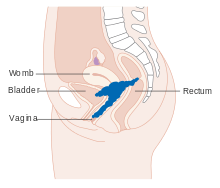
Stage 4A cervical cancer
-

Stage 4B cervical cancer
Treatment is individualised to the patient, her age, reproductive goals, functional status, and access to health care resources.
Treatment according to the FIGO stages of cervical carcinoma
Stage Ia1- therapeutic conization in young individuals, extrafascial hysterectomy in post reproductive age
Stage Ia2, Ib1, Ib2 and IIa- warthein's radical hysterectomy
Stage IIb, IIIa, IIIb and IVa- Generally chemoradiotherapy (cisplatin is used as radio sensitiser) is used. Surgery is not offered to this group of women because of the significant risk of positive margins and positive nodes.
Stage IVB and recurrent cancer- Palliative therapy (also depends on previously used treatments).
External links
- FIGO Committee on Gynecologic Oncology (2006-10-10). "Cancer of the Cervix Uteri: 3.1 Staging". Staging Classifications and Clinical Practice Guidelines for Gynecological Cancers (PDF) (3rd ed.). International Federation of Gynecology and Obstetrics. pp. 37–41. External link in
|publisher=(help)
Originally published as Benedet JL, Bender H, Jones H, Ngan HY, Pecorelli S (August 2000). "FIGO staging classifications and clinical practice guidelines in the management of gynecologic cancers. FIGO Committee on Gynecologic Oncology". Int J Gynaecol Obstet. 70 (2): 209–62. PMID 11041682.